24 Sep Importance of Colonoscopy in Gastroenterology
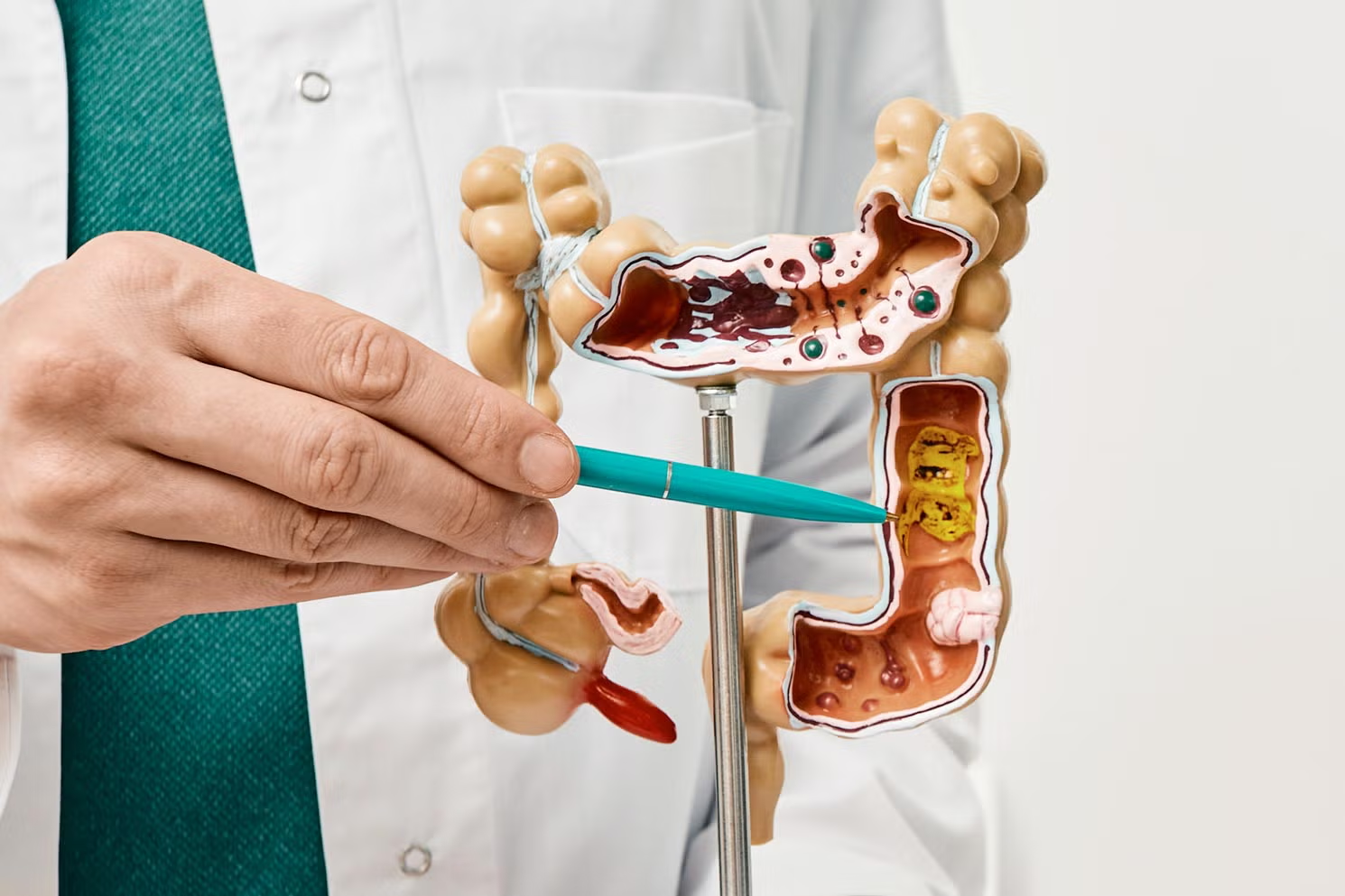
Colonoscopy is one of the most valuable tools in gastroenterology. It is a medical procedure that allows doctors to directly examine the inside of the large intestine (colon) and rectum using a long, flexible tube equipped with a camera. While many people feel nervous or even embarrassed about undergoing this test, it plays a crucial role in detecting, diagnosing, and preventing many serious conditions, including colorectal cancer.
In this article, we’ll break down why colonoscopy is important, what it involves, how it benefits patients, and why doctors in gastroenterology recommend it so often.
What is a Colonoscopy?
A colonoscopy is a procedure performed by a gastroenterologist to check for abnormalities in the colon and rectum. The instrument used, called a colonoscope, has a small camera at the tip. This camera transmits real-time images to a monitor, allowing the doctor to carefully examine the lining of the bowel.
The procedure usually takes about 30 to 60 minutes. Patients are given sedation so they remain comfortable throughout. During the exam, doctors can:
- Detect and remove polyps (small growths that can develop into cancer).
- Identify ulcers, tumors, inflammation, or bleeding.
- Collect tissue samples (biopsies) for further testing.
Why Colonoscopy is Important in Gastroenterology
1. Early Detection of Colorectal Cancer
Colorectal cancer is the second leading cause of cancer-related deaths worldwide. The good news is that it often develops slowly over many years, starting as small, benign polyps. Colonoscopy allows doctors to detect these polyps early and remove them before they turn into cancer. This makes colonoscopy not just a diagnostic tool but also a preventive one.
2. Diagnosis of Digestive Disorders
Colonoscopy helps gastroenterologists diagnose conditions such as:
- Inflammatory Bowel Disease (IBD), including Crohn’s disease and ulcerative colitis.
- Diverticulosis and diverticulitis.
- Unexplained chronic diarrhea or constipation.
- Rectal bleeding.
By identifying the root cause of digestive symptoms, doctors can create more effective treatment plans.
3. Prevention Through Polyp Removal
Unlike many medical tests, colonoscopy is both diagnostic and therapeutic. If a gastroenterologist sees polyps, they can remove them immediately during the same procedure. This step alone prevents countless cases of colorectal cancer every year.
4. Monitoring Existing Conditions
For patients with a history of colon cancer, polyps, or inflammatory bowel disease, regular colonoscopies are essential. They allow doctors to monitor changes, catch recurrences early, and adjust treatments accordingly.
5. Peace of Mind for Patients
Many people experience digestive symptoms like bloating, rectal bleeding, or changes in bowel habits. A colonoscopy can provide answers and rule out serious diseases. This reassurance is often just as important as treatment.
Who Should Get a Colonoscopy?
Medical guidelines generally recommend that adults begin regular colonoscopy screenings at age 45. However, some individuals may need earlier or more frequent testing, including:
- Those with a family history of colorectal cancer or polyps.
- Patients with chronic digestive conditions such as Crohn’s disease or ulcerative colitis.
- People with genetic conditions like Lynch syndrome or familial adenomatous polyposis.
- Anyone experiencing concerning symptoms such as unexplained bleeding or persistent abdominal pain.
What Happens During a Colonoscopy?
- Preparation (Bowel Prep) – A clean colon is crucial for accurate results. Patients are asked to follow a clear liquid diet and take prescribed laxatives the day before.
- Sedation – To ensure comfort, patients receive sedation through an IV. Most people remember little or nothing about the procedure.
- Examination – The doctor inserts the colonoscope into the rectum and advances it through the colon while viewing images on a screen.
- Polyp Removal or Biopsy – If polyps are found, they are removed. Suspicious areas can be biopsied.
- Recovery – Patients usually rest for an hour after the procedure until the sedation wears off.
Benefits vs. Risks
Like all medical procedures, colonoscopy has benefits and some risks.
Benefits include:
- Early cancer prevention.
- Accurate diagnosis of digestive problems.
- Immediate treatment through polyp removal.
- Peace of mind with clear results.
Risks include:
- Rare complications like bleeding or perforation of the colon.
- Mild discomfort from preparation.
- Temporary bloating or cramping after the procedure.
The benefits, however, far outweigh the risks, especially for individuals at higher risk of colon disease.
Colonoscopy vs. Other Screening Tests
There are other methods for colon cancer screening, such as stool tests (FIT, FOBT), CT colonography, and flexible sigmoidoscopy. While these can be useful, they have limitations. For example:
| Screening Test | Detects Polyps? | Requires Prep? | Can Remove Polyps? | Frequency |
|---|---|---|---|---|
| Colonoscopy | Yes | Yes | Yes | Every 10 years (if normal) |
| Stool-based Tests (FIT/FOBT) | No (only detects blood) | No | No | Every 1 year |
| CT Colonography | Yes | Yes | No | Every 5 years |
| Sigmoidoscopy | Yes (limited to lower colon) | Yes | Yes (partially) | Every 5 years |
Colonoscopy remains the gold standard because it not only detects problems but also treats them in the same session.
Overcoming Fear and Stigma
Many people avoid colonoscopy because of fear, embarrassment, or myths about discomfort. The truth is:
- Sedation makes the procedure almost painless.
- Doctors and nurses perform colonoscopies daily with professionalism.
- The preparation is temporary but the benefits are lifelong.
Spreading awareness about the importance of colonoscopy in gastroenterology can encourage more people to undergo screening and save lives.
Conclusion
Colonoscopy is a cornerstone of gastroenterology. It saves lives by detecting colorectal cancer early, helps diagnose digestive disorders, and prevents disease through polyp removal. Though many people fear the procedure, it is safe, effective, and essential for long-term digestive health.
If you are due for a screening, don’t delay. Talk to your doctor and take this important step toward protecting your health.
FAQs
1. How often should I get a colonoscopy?
Most adults should get one every 10 years starting at age 45, but those with risk factors may need more frequent testing.
2. Is a colonoscopy painful?
No, most people receive sedation and do not feel pain. Some mild cramping or bloating afterward is possible.
3. What happens if a polyp is found?
The doctor usually removes it immediately during the colonoscopy. The tissue is then tested in a lab.
4. Can I go to work the next day?
Yes, most patients can resume normal activities the following day, but driving on the same day is not recommended because of sedation.
5. Are there alternatives to colonoscopy?
Yes, stool tests and CT colonography are options, but they are less comprehensive. Colonoscopy remains the gold standard for both detection and prevention.

No Comments